COVID-19 has exposed the challenges U.S. hospitals face when responding to peak surges in demand. Anthony Roesch, director of HOK’s Healthcare Consulting group, and Anthony Rosania MD, MHA, an emergency physician and member of the Healthcare Consulting team, believe a coordinated and flexible approach to healthcare delivery—modeled after an energy grid—is needed to address future crises and long-term resilience of the nation’s healthcare system.
Over the past two decades, U.S. hospital systems have consolidated operations into a hub-and-spoke model of care delivery. This market-driven approach has created efficiencies within hospital networks while exposing dangerous vulnerabilities and inequities when faced with sudden demands like the coronavirus pandemic.
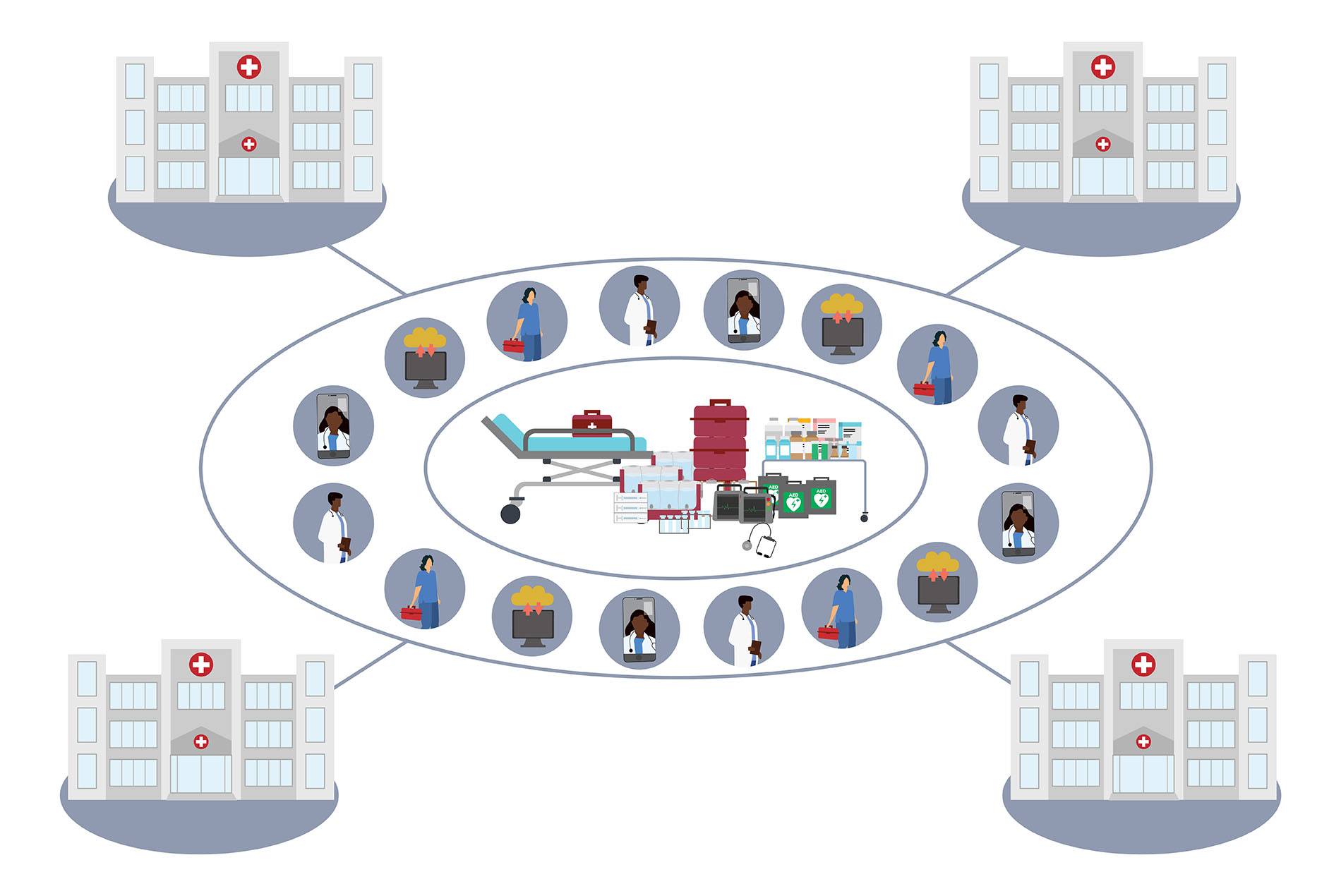
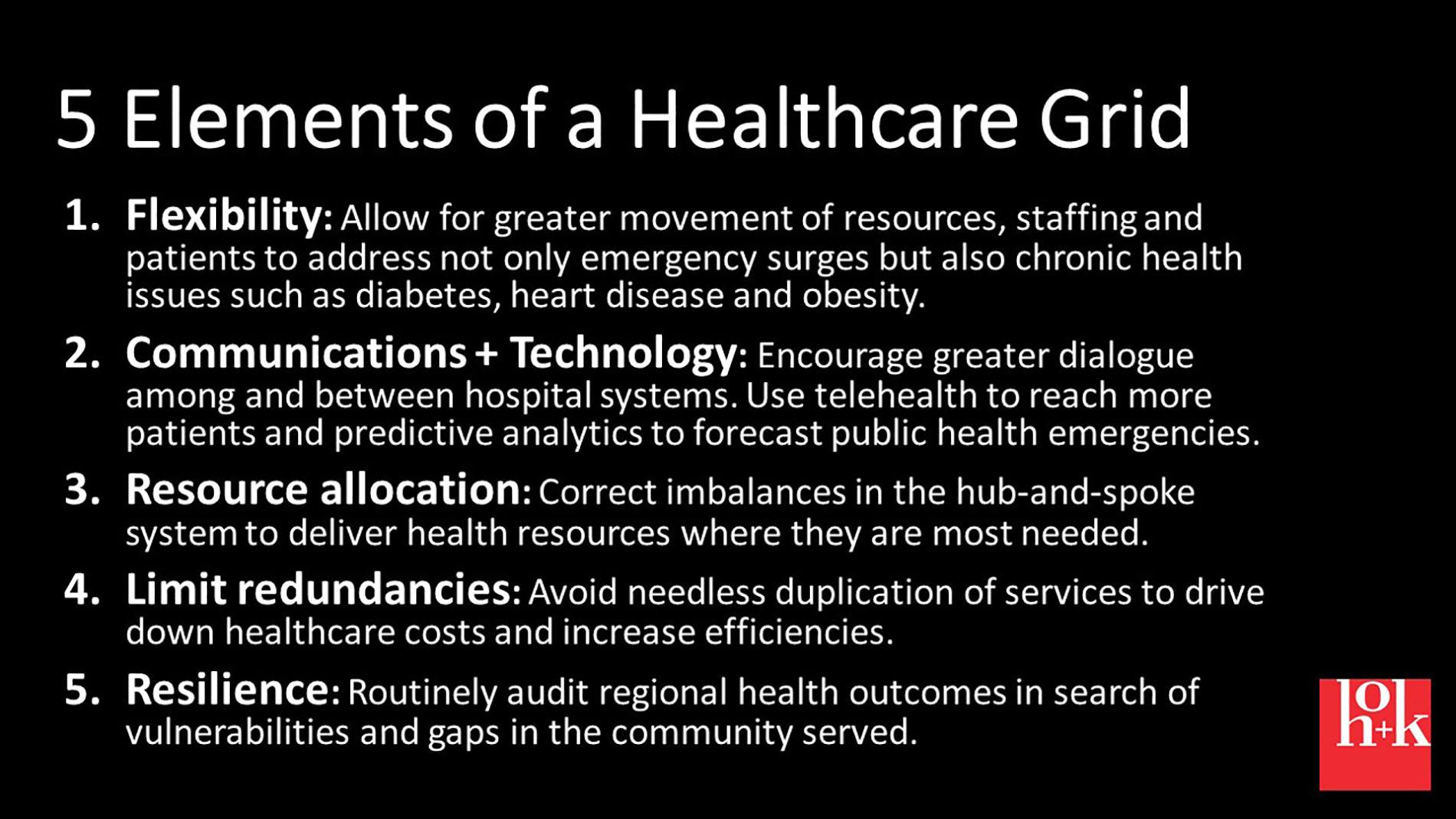
In this Q+A, HOK’s Roesch and Rosania explore a more resilient model of healthcare delivery that takes its cues from the backup systems inherent in power grids. Such a system would enhance flexibility, communications, resource allocation and resilience across hospital networks. It also would reduce redundancies and spending.
The two of you have been examining the idea of a “health grid” from different perspectives. Could you explain your vision?
Roesch: One could be skeptical of a power grid analogy when sometimes the power goes out. We would never want that to happen in our hospitals. But it almost happened when COVID-19 hit last spring. Applying a grid, or failsafe, system to healthcare is something I’ve been thinking about while working for public health systems for the last 20 years.
Why aren’t hospitals operated more like public utilities instead of individual entities? Hospitals are essential public utilities. As we’ve witnessed, you can’t turn them off like you can a movie theater or restaurant. Why aren’t they regulated to prevent situations like we had in New York, where a hospital in Queens can’t keep up with a surge while resources are available in Manhattan hospitals?
A health grid would encourage hospital systems to coordinate with each other during times of crisis. In normal times, it would avoid redundancies and ensure adequate combined resources for an entire region.
Rosania: As an emergency department administrator, I’ve been thinking about how a grid would help individual health systems. During this pandemic, the problem for many hospitals wasn’t that they didn’t have enough space to treat patients. It was a shortage of the right types of spaces and the people and resources required to turn those spaces into effective treatment areas for our most critically ill. Due to a lack of other resources in some hospitals, entire floors went empty during the COVID-19 surge. The biggest challenge was finding enough skilled nurses and doctors to care for the sickest patients. Hospitals could then find themselves competing with one another, or even government entities, for the same resources. This happened with field hospitals that were underutilized during the height of the crisis.
When I think of a health grid, I think of how a hospital or a health system that runs multiple hospitals can create a plan for responding to a surge without having a situation like in New York or Houston, where hospitals struggled to keep up. The development of microgrids within our larger systems could help create a cultural and mental shift that moves us toward the ultimate goal of a national health grid.
How would these grids work across multiple health systems and within a single hospital network?
Roesch: Though healthcare in many parts of the U.S. is oversaturated, that capacity isn’t necessarily in the right places. Hospital systems have increasingly adopted a hub-and-spoke model in which the bulk of regional hospital resources are centrally located in a flagship or hub facility. The decision to operate this way is almost always based on efficiency and market penetration. Yet for the most part, healthcare isn’t a market-driven industry. It’s disease-based. Unlike when they’re going to a restaurant or store, not many people wake up saying, “Which hospital should I choose today?”
“Hospitals are essential public utilities. You can’t turn them off like you can a movie theater or a restaurant.”
I’m proposing that hospitals and health systems better distribute their critical resources—infrastructure, equipment, staffing—to meet public health needs. Just as an electric grid ensures that the power doesn’t go out during peak demand, a health grid would allow hospitals to better accommodate surges. It would mean that if a large healthcare provider wanted to add intensive care beds to its flagship hospital, it would first need to consider the capacity across the region. Could those beds be put to better use in a location less capable of handling a sudden rise in demand? The idea of what should work in the throes of a pandemic should also work with other health issues, such as treating diabetes or heart disease.
Rosania: Looking at this for a single hospital network, the focus needs to be on staffing and effectively using the available space. Healthcare is incredibly siloed. An ICU nurse is an ICU nurse. A same-day surgery nurse is a same-day surgery nurse. It’s true that each specialty requires a specific expertise, but many skills are transferable. In a surge like we had with COVID-19, there’s no reason why a same-day surgery nurse, ear-nose-throat physician or other specialized caregiver couldn’t help in the ICU. At the very least these people could assist the ICU attendant with non-critical checks and procedures.
We already ask residents—physicians still in training who have just a year or two of experience—to rotate between specialties and care areas. It’s counterintuitive to think that we can’t use physicians from other specialties as extenders in the same way.
There are challenges to safely making this a reality. Yet if we don’t create resilience at this hospital level, we will have skilled caregivers sitting on the sidelines during surges and thus remain vulnerable during public health crises.
Some might argue that a health grid takes away choice or somehow “socializes” medicine? How do you respond to that?
Roesch: Most of our health system is either publicly funded or insured through programs like Medicare. In the 1970s and continuing through the 1990s, state-backed Certificate of Need (CON) regulations tried to address disparities. These regulations, which were primarily intended to prevent unnecessary costs, have either been watered down or eliminated.
The inpatient care we’re talking about impacts 10 to 12 percent of our total healthcare encounters but adds up to much more in terms of total healthcare spending. The larger percentage of care encounters—such as primary care, specialty services, mental health, long-term care and other outpatient offerings—respond more to market forces. Yet to improve overall public health, their inclusion is integral to the success of the health grid.
Rosania: If there is any take-home message from this pandemic, it is that healthcare is a public trust. We need to start treating it like one. The issues we’re discussing—ingrained system-level problems—have put people’s lives at risk. A flexible, affordable, resilient healthcare system is a matter of public interest and arguably a matter of national security. We must be open to real solutions without getting caught up in political debates, which is easier said than done.
“A flexible, affordable, resilient healthcare system is a matter of public interest and arguably a matter of national security.”
One way to allay those concerns would be to clearly delineate triggers for resource sharing and reallocation. Take credentialing, for example. I appreciate the desire for systems and hospitals to have some control over their credentialing processes. But during a crisis, it should be possible to enact emergency credentials that allow healthcare workers to provide care in any setting or system. I think most healthcare executives would like a system that enables them to quickly call in resources. By putting clear guardrails in place to ensure equitable sharing and prevent misuse—such as restrictions on poaching these emergency staff workers—we could alleviate concerns about the over-socialization of resources.
How could a grid benefit a rural hospital or medical provider?
Rosania: A grid would allow medical services to more easily transfer to rural areas. It’s almost always faster and cheaper to deliver a doctor to a patient than it is to transfer a patient to a doctor. Value is created for everyone in that scenario—provided the rural hospital has the equipment necessary to treat the patient.
Roesch: This also is where telehealth comes into play. The health grid is as much about moving information and technology through the system as it is the physical resources.
Rosania: Assuming the patient doesn’t need surgery, a specialist doctor could consult with a patient via telemedicine from anywhere in the health grid and, with the help of an in-person medical assistant or primary care physician, perform many diagnoses and follow-ups. Other technologies, such as remote monitoring equipment and smart pumps to deliver exact doses of medications, makes this type of long-distance care possible. Telehealth is a force multiplier in terms of allowing us to treat more patients.
How does design factor into the health grid? And what are the next steps to seeing something like this materialize?
Roesch: The health grid begins with design-responsive infrastructure. From a regional approach, it requires a comprehensive look at the current needs and resources and mapping out areas where there are gaps in coverage or an overabundance of supply. Ultimately, a health grid—like a public utility—would require some type of oversight body. For now, it’s important to open up this idea for dialogue. We need to take a hard look at how we’re pricing and building up healthcare. With a grid system, there are real upstream and downstream benefits.
Rosania: From an intrasystem perspective, the design work begins with an inventory of a health network’s current space and staffing and then looks at how those resources can be used more effectively to address surges.