Karen Pottebaum, Kathleen Schwarz and Nupur Gupta of HOK’s Healthcare group share why they’re passionate about designing oncology spaces and how planning and design can improve the experiences of patients and staff.
The world is rapidly changing. So, too, is cancer care. Today’s oncology centers must keep pace with evolving technologies and medical advancements while also integrating new healthcare protocols and restrictions. In this Q+A, members of HOK’s Healthcare team share their thoughts on designing cancer care facilities with flexibility to accommodate unforeseen challenges like COVID-19.

L-R: Karen Pottebaum, Kathleen Schwarz, Nupur Gupta
What excites you about cancer care design?
Kathleen Schwarz (Senior Healthcare Consultant): We’re seeing an evolution in cancer care. It used to be more of a one-size-fits-all approach to care delivery. Today it is targeted and personalized and constantly changing. Many patients are now living for 10, 15, 20 years and longer following their initial diagnosis. Meeting those patients along the care continuum is important. Cancer care is increasingly delivered outside the four walls of the hospital. Thinking about how to provide service and treatment in a variety of environments is exciting.
Nupur Gupta (Medical Planner): What excites me the most is to see ambulatory care facilities providing different cancer treatment options outside the hospital environment. Cancer treatment options have evolved over the years—from chemotherapy to linear accelerators to brachytherapy and now MR-Linac technology. Often the equipment required for radiation treatment is quite large and can intimidate patients. It’s important to think about how we can design an environment that puts patients at ease during the treatment. The treatment rooms are often equipment-dominated, but there are options for creating a calming environment.
Karen Pottebaum (Senior Medical Planner): What excites me is more futuristic. I’ve had the opportunity to talk with researchers working on new treatments like nanotechnology that promise significant benefits with targeted treatments that do less damage to the body. Though we are probably looking at another 10 years before we see a wider implementation of this treatment, it will provide more outpatient options as it changes how providers prescribe care.

A bright, open lobby welcomes patients and their families to the NewYork-Presbyterian David H. Koch Center in Manhattan. Locating the infusion and radiation oncology services on the 4th floor provides patients access to city views and natural light.
How can design support the emotional journey of patients?
Kathleen: By making sure it’s a seamless experience without duplication. It’s important to consider the different patient types throughout the process. If we’re talking about pediatric patients, what can we do to meet their needs when they are waiting for an appointment? For older patients, how can we help them navigate the process if they require assistance? When we think about design or planning efforts, we want patient consultations to happen within a dedicated quiet area where patients can have conversations to address questions about their treatment, their well-being and anything else that is concerning them. Most of the time patients are coming in for radiation treatments on a daily or weekly basis, so they’re frequently visiting the space. How can the design help them get in and out quickly and easily?
Karen: Cancer patients often feel so much is out of their control. If we can give them the ability to take some control, their experiences will be more positive. If you’re a patient getting daily treatment, the ability to check yourself in and get to your appointment without having to go through the whole check-in process is appreciated. When you’re going through radiation treatments, you’re often feeling unwell and sickly. During this time, having exposure to a nutritionist or amenities like a spa or aromatherapy can make the experience more positive.
Nupur: Technology that empowers patients to control their physical environment can bring a positive change. Something as simple as giving patients control of their lighting choices within a treatment room makes a difference. We’ve designed treatment and diagnostic rooms in which patients can change the lighting levels to fit their mood and even display motion imagery on the ceiling and wall of their choice. Children particularly enjoy being able to control their environment.
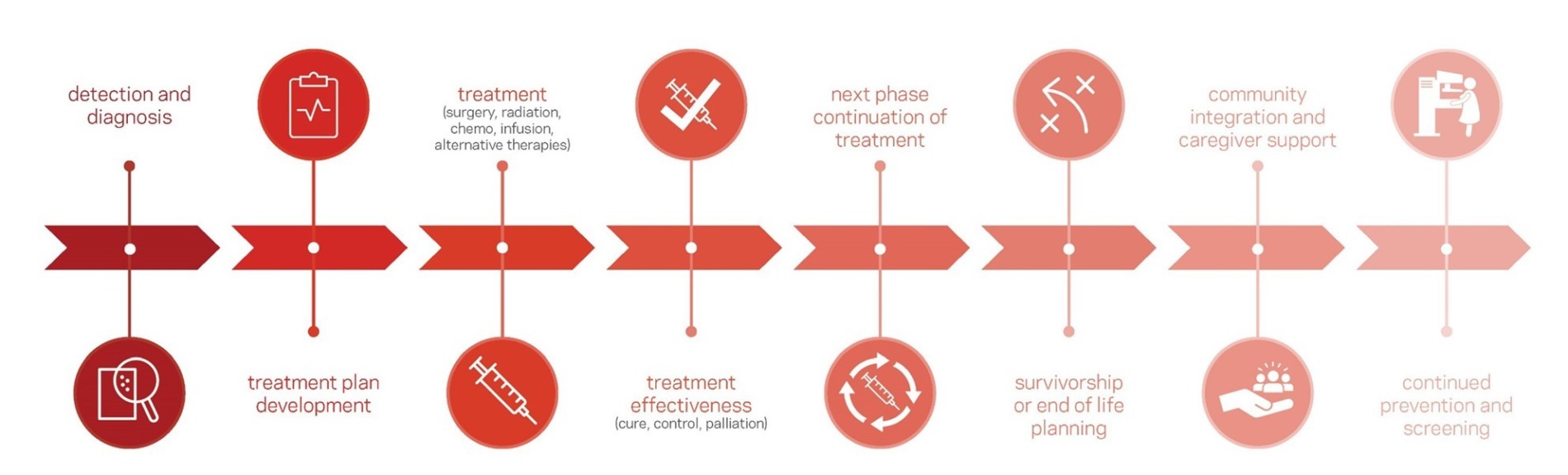
The care journey for cancer patients involves numerous steps spread over months and years, requiring designers to consider ways to make treatment and recovery as streamlined and comfortable as possible.
How can cancer design assist caregivers in their jobs?
Karen: Designers and planners tend to underestimate the amount of space that the staff needs, particularly when it comes to collaboration and teamwork. Cancer care is a team effort. One of the chief complaints I hear from staff is they don’t have enough space to work in the treatment area. They need team rooms and enlarged consult rooms, especially in teaching hospitals. Just having space where staff can have private conversations or interact with researchers, nutritionists and other ancillary specialists is important. Often there is no spot for all these people to work within the treatment area, so everyone is ganged up at the nurse’s station, which is the least-private area.
Kathleen: Many treatment centers lack dedicated space required for clinical trial teams or specialized services. This hinders the ability of those caregivers to deliver quality care. Space planners and designers need to accommodate the more complex patient visits. The oncology care team requires dedicated space for respite outside of patient-facing areas for wellness and as a place where they can recharge.
Nupur: During a project’s design phase, it’s crucial to consider creating staff spaces that provide flexibility and accommodate different workplace settings. In some facilities, decentralized stations are best. For others, collaborative areas work better. Staff should be able to control what works best for their team. It helps the staff when the workplace provides different options for collaboration as well as individual work stations or “hot desks.” It’s a challenge that requires lots of thought and collaboration during design.

Daylight permeates the Ohio State University Comprehensive Cancer Center and helps support the physical and mental well-being of patients. A terrace, garden and café on the 14th floor offers visitors and staff additional connection to the outdoors.
How might the coronavirus pandemic impact cancer care going forward?
Nupur: COVID-19 has increased anxiety in patients who are already under a lot of stress due to their health condition. We can alleviate some of that anxiety by providing clear wayfinding. With COVID-19, facilities are requiring additional protocols at arrival that increase confusion among patients. Thinking about clear directions even before the patient enters the building—things like where to park, where to enter and how to navigate to the check-in desk—will help tremendously. The design of waiting areas should include different seating options that put patients at ease based on their choices. Technology is also playing a role. For example, facilities are exploring options where imaging and radiation treatment are done at the same time, which cuts down the number of visits.
Karen: I’ve gotten requests to redesign staff work areas in response to coronavirus. As much as the patients need to be socially distancing, so does the staff. Rather than having centralized staffing, we’re looking at more decentralized satellite stations that allow staff to communicate while keeping them somewhat apart. It’s an iterative process in which everyone is learning as we go.
Kathleen: It will have a long-term impact on the patients’ emotional journeys. An important part of cancer care has been allowing patients to bring family members and friends to their treatments, especially for infusions that can last hours. Now patients will likely have to make that journey by themselves or with—at most—just one support person. We need to think about how design can make that journey as comfortable, intuitive and expedient as possible. COVID-19 is forcing designers, planners and clients to think more proactively. Yes, the changes we are making now are a reaction to the coronavirus. But they are also anticipating the challenges of future pandemics and other crises.
Top image: Treatment rooms with programmable lights and displays at the University of Texas MD Anderson Cancer Center in Houston. Photo: Dror Baldinger.
